Abstract
Background: High- risk multiple myeloma (MM) is considered challenging to treat because of the risk of early relapse and increased mortality. The main factors contributing to high risk myeloma are poor prognostic cytogenetic abnormalities that include 17p deletions, 1q21 gains, 1p deletion, t (4;14), t (14;16), and t (14;20). Other features of high risk MM include extramedullary disease (EMD) which is associated with an adverse prognosis in newly diagnosed and in relapsed MM patients with overall survival of less than 6 months. Another entity of high risk MM is primary plasma cell leukemia (pPCL) and has a very poor prognosis. Our institution performed a retrospective review that included induction/salvage therapy using multi-agent chemotherapy with novel agents such as a proteasome inhibitor and an immunomodulator agent (Imid) to achieve a better overall response rate.
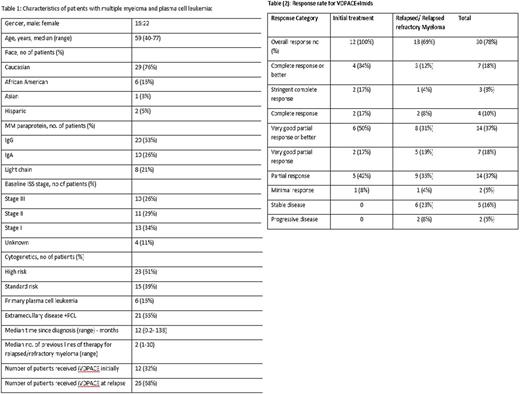
Patients & Methods: Thirty eight patients with MM, primary plasma cell leukemia, and myeloma with EMD between January 2012 and June 2017 at the University of Kansas Health System were reviewed These patients received VDPACE consisting of bortezomib 1 mg/m2 subcutaneous (SC) on days 1,4,8 and 11, doxorubicin 10 mg/m2 continuous infusion (CI) x 4 days, cisplatin 10 mg/m2 CI x 4 days, Cyclophosphamide 400 mg/m2 CI x 4 days, etoposide 40 mg/m2 CI x 4 days, an Imid either thalidomide 200 mg for 4 days or lenalidomide 25 mg for 14 days or pomalidomide 4 mg for 14 days every 28 days. Descriptive analyses were performed on available data for patient characteristics, disease course, and outcomes. Responses were evaluated using the IMWG criteria.
Results: The median age was 59 years (40-77) for those who received VDPACE + Imid, 53% of patients had IgG isotype, 26% had ISS stage III at diagnosis, 61% had high risk cytogenetics, 55% had EMD and pPCL. Median number of cycles of VDPACE+ Imid received was 1 (1-4) cycles. Thirty patients (68%) received treatment for relapsed disease. In the relapsed group, the median prior lines of therapy were 2 (1-10), 100% had received proteasome inhibitor, 88% had received an Imid and 73% had received autologous stem cell transplant (ASCT), median number of ASCT prior to treatment was 1 (0-3). The ORR was 69%. Twelve patients (32%) received treatment as initial therapy with an ORR of 100%, 6 of these patients (16%) had pPCL. The response rates are summarized in table 2. The response rate for patients who had EMD+pPCL was 80% with 48% who achieved VGPR and better. Twenty-two patients (58%) proceeded with consolidation therapy with ASCT or allogenenic stem cell transplant (AlloSCT).
Conclusion: Our single institution experience shows that patients with high risk MM, EMD and pCNS can achieve a significant response rate using VDPACE+Imid. This proves VDPACE+Imid can be utilized as salvage therapy in relapsed MM and as an initial therapy in pPCL and EMD. However, we believe that this treatment followed by high dose chemotherapy with ASCT should be further studied in terms of deeper response and OS to identify the long term clinical benefits of the treatment.
Ganguly: Amgen: Other: Advisory Board; Seattle Genetics: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal